
These efforts include, but are not limited to, completion of a Coordination of Benefits form and/or signing Release of Information forms. It is important that you cooperate with CHP in any efforts made to obtain such information. This could include details regarding other Health Care or accident coverage you may have. There may be situations when, in order to process your request, CHP will need additional information.
Fl bcbs timely filing requirements code#
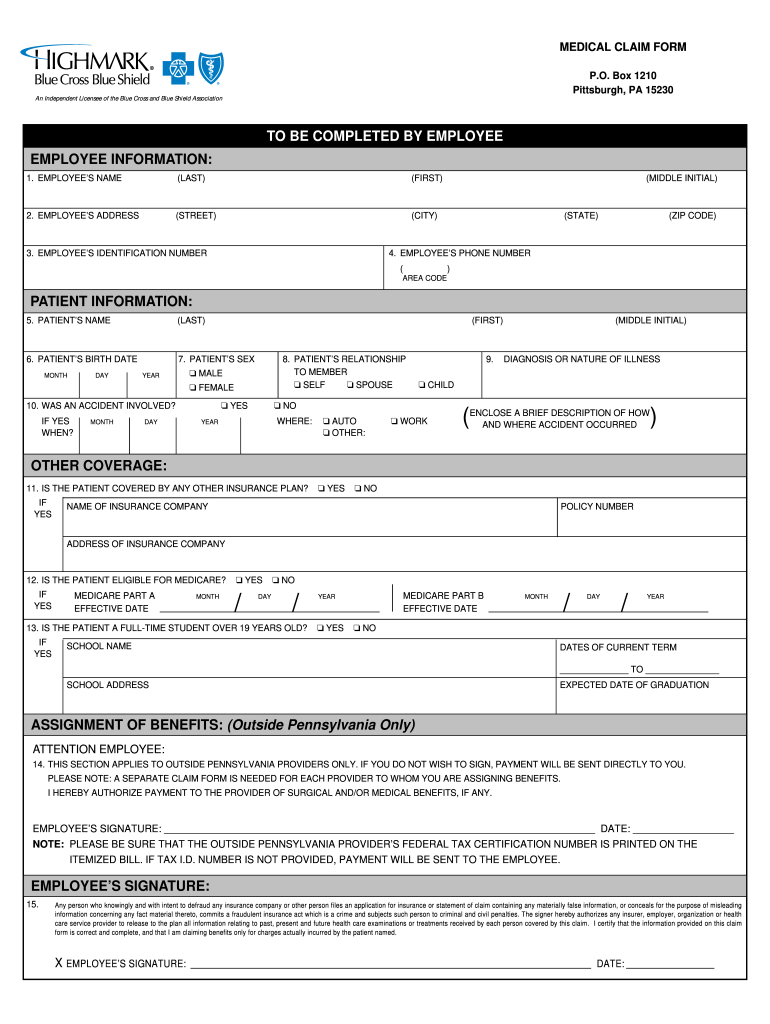
A copy of the billing statement reflecting the CPT codes and Diagnosis Code information.A claim form, located here: Reimbursement Form.To ensure a request for reimbursement is processed efficiently and accurately, the request must include the following: In any event, any claim for payment or reimbursement submitted by a member must be submitted no later than one (1) year after the date service(s) were rendered unless the member was legally incapacitated. If it is not reasonably possible to submit a claim in the time required, CHP will not reduce or deny the claim for this reason if proof is filed as soon as possible. Any time you receive a bill, or request reimbursement for a payment you have already made, you must submit these claims to CHP's Claims Department within six (6) months from the date service(s) were rendered. There may also be a time when you feel a deductible, copayment, or co-insurance amount should not apply. These could include emergency services or services received from non-contracted, out-of-network doctors or providers. There may come a time when you are billed for services you believe should have been covered by CHP or you are asked to pay for services at the time they are rendered.
If I am billed for a service that I think CHP should pay, what do I do? For specific estimates, unique to your situation and deductible status, you can contact CHP's Member Services Department via email at or via telephone at (850) 383-3311, 8:00 am - 5:00 pm, Monday - Friday How can I find out how much a service or procedure will cost if I have not yet met my deductible?įor medical service cost estimates, we recommend you use a helpful online tool called Fair Health. Balance billing may be waived for emergency services received at an out-of-network facility. In cases like these, you will be responsible for paying for what your plan does not cover. Charging this extra amount is called balance billing. Depending on the health care professional, the service could cost more or not be paid for at all by your plan.
Fl bcbs timely filing requirements professional#
A health care professional who is out of your plan network can set a higher cost for a service than professionals who are in your health plan network. Out-of-network services are from doctors, hospitals, and other health care professionals that have not contracted with your plan. What is meant by out-of-network liability and balance billing? What you need to know about using your Capital Health Plan (CHP) benefit plan


 0 kommentar(er)
0 kommentar(er)
